Surgery for spinal fractures restores stability and protects the spinal cord, but the operation is only the beginning of recovery. The path to regaining mobility and independence depends heavily on rehabilitation. Dr. Larry Davidson, a board-certified neurosurgeon, with fellowship training in complex spinal surgery, has emphasized that physical therapy is not a secondary phase of treatment, but is a central component. Without structured rehabilitation, surgical corrections may not translate into meaningful functional gains.
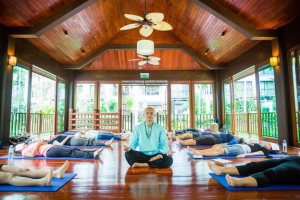
Rehabilitation after spinal fracture surgery is designed to restore strength, rebuild endurance and help patients adapt to the changes in their spines. From the first steps taken after surgery to long-term therapy, this process shapes outcomes and determines whether patients can confidently return to their normal activities.
Early Post-Operative Rehabilitation
The first stage of rehabilitation begins almost immediately after surgery. Once the patient is stable, physical therapists encourage gentle movements and assisted walking. Early mobilization reduces the risk of complications such as blood clots, pneumonia or muscle waste. It also promotes circulation, which supports healing around the surgical site.
Therapists guide patients in performing movements safely, showing how to sit, stand and lie down, without putting stress on the spine. These basic skills form the foundation for further progress. Pain management, through medications and guided exercises, is incorporated to help patients stay actively engaged in their recovery.
Building Strength and Endurance
As patients progress, therapy shifts toward rebuilding muscle strength. Core muscles are especially important because they support spinal alignment and reduce stress on surgical repairs. Targeted exercises gradually increase intensity, helping patients restore balance and stability.
Endurance training is equally vital. Walking programs, stationary cycling and aquatic therapy are often introduced to improve cardiovascular health, while minimizing impact on the spine. These activities help patients build stamina for daily tasks, setting the stage for greater independence.
Restoring Mobility and Flexibility
Mobility exercises are tailored to each patient’s needs. Stretching routines improve flexibility in the hips, legs and shoulders, supporting smoother movement and reducing compensatory strain on the spine. Gentle range-of-motion exercises are introduced early and gradually expanded as healing progresses.
Therapists also address posture, teaching patients how to move with alignment that supports both comfort and long-term spinal health. For those who had deformities corrected during surgery, learning to adjust to a new spinal posture is an essential part of rehabilitation.
Adaptive Training for Daily Activities
Rehabilitation goes beyond exercise. Occupational therapists work alongside physical therapists to help patients adapt to daily tasks, such as lifting objects, climbing stairs or dressing. Training includes safe body mechanics, reducing the risk of reinjury or stress on healing structures. Patients are also educated in ergonomics, including proper chair support, mattress choice and safe techniques for bending and reaching. These strategies protect the spine in everyday life and help prevent setbacks.
Addressing Neurological Deficits
In some cases, spinal fractures involve neurological injury. Rehabilitation must then address not only mobility but also coordination, sensation and muscle control. Therapists use targeted exercises, functional electrical stimulation and balance training to maximize neurological recovery. Surgery relieves pressure on the spinal cord, and rehabilitation helps patients translate this into functional improvement. By engaging both the nervous and musculoskeletal systems, therapy supports comprehensive healing.
Pain Management in Rehabilitation
Pain is a common challenge during recovery, but effective management helps patients stay active in therapy. A combination of approaches, including medication, guided movement and non-drug techniques like heat, ice and massage, can be used. Physical activity often eases pain over time by strengthening muscles, improving posture and reducing strain on the spine. Patients are encouraged to see movement as an important tool for pain control, complementing, rather than replacing, medication.
The Role of Patient Engagement
Successful rehabilitation depends heavily on patient participation. Exercises performed in therapy sessions must be continued at home to reinforce progress. Consistency builds strength and mobility more effectively than intermittent effort. Education is a critical part of this process. Patients who understand the purpose of each exercise are more likely to remain committed. Motivation and adherence are often the deciding factors in long-term outcomes.
Dr. Larry Davidson notes, “Recovery is a process, and every step forward matters.” In rehabilitation, this emphasizes that while regaining function takes ongoing effort, each milestone builds confidence and moves patients closer to full independence.
Athletes and Rehabilitation Strategies
Athletes recovering from spinal fracture surgery face unique demands. Their rehabilitation programs are more intensive, focusing on restoring strength, flexibility and performance-specific skills. Therapists design exercises that simulate sport-related movements, gradually preparing athletes to return to competition. Aquatic therapy, resistance training and plyometric exercises are often incorporated as healing progresses. Close monitoring helps patients work toward performance goals, while keeping the spine protected.
Advances in Rehabilitation Tools
Technology is expanding the tools available in rehabilitation. Wearable devices now track posture, activity levels and progress in real time, providing both patients and therapists with actionable feedback. Robotics and exoskeletons are being tested to assist in walking programs, particularly for patients with neurological deficits.
Virtual reality is also being explored as a motivational tool, offering engaging environments that encourage patients to complete exercises. These innovations complement traditional therapy, making rehabilitation more effective and accessible.
Long-Term Rehabilitation and Maintenance
Rehabilitation does not end when patients leave formal therapy. Long-term maintenance is essential to preserving gains in mobility and preventing future fractures. Regular exercise routines, continued core strengthening and healthy lifestyle choices, such as nutrition and fall prevention, all play roles in sustaining progress. Ongoing follow-up with therapy teams allows for adjustments as patient needs develop. By treating rehabilitation as a lifelong commitment, rather than a short-term process, patients protect their spinal health for the future.
The future of spinal fracture rehabilitation is likely to integrate even more personalized strategies. Advances in biologics may accelerate healing, allowing therapy to begin sooner. Wearables and AI-driven feedback systems will provide tailored exercise plans that adjust in real time. These tools will enhance the partnership between surgeons, therapists and patients, helping to make sure that rehabilitation reflects both medical expertise and individual goals.
Rehabilitation after spinal fracture surgery is a critical phase of care, turning surgical corrections into meaningful functional outcomes. Through physical therapy, strength and endurance are rebuilt, mobility is restored, and patients learn to adapt safely to daily life. The approach underscores that recovery is not defined by the operation alone, but by the effort invested in therapy afterward. This work highlights the central role of rehabilitation in giving patients the confidence, independence and mobility they need to move forward after spinal injury.












Add Comment